 Definition: Orthostatic hypotension (OH) is a form of low blood pressure that occurs with positional change (i.e. sitting up from lying down, standing up from sitting). It is commonly used for the diagnosis of volume depletion
Definition: Orthostatic hypotension (OH) is a form of low blood pressure that occurs with positional change (i.e. sitting up from lying down, standing up from sitting). It is commonly used for the diagnosis of volume depletion
Orthostatic Vital Signs
- A reduction of systolic blood pressure (SBP) of at least 20 mm Hg
- A reduction in diastolic blood pressure (DBP) of at least 10 mm Hg
- An increase in heart rate (HR) by > 30 beats per minute
One of the above criteria must be met while measured 3 minutes after standing from a supine position.
Clinical Question: Are orthostatic vital signs useful in finding patients with occult volume loss? Do they add to our standard clinical assessment of patients?
Review of the Evidence
Background on Orthostatics
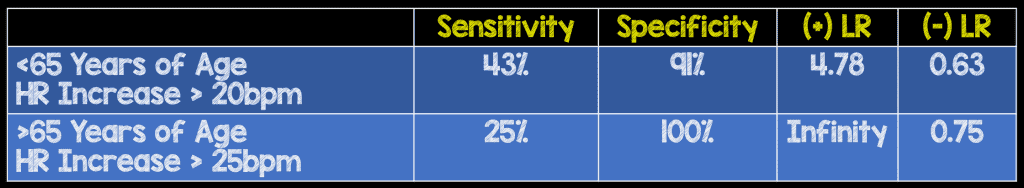
- The development of orthostatic criteria appear to be derived from measuring blood pressure and HR before and after young, healthy patients donate blood
- Baseline OH in Adolescents
- Orthostatic HR changes common (Skinner 2010)
- Transient OH common (Stewart 2002)
- Blood pressure changes usually fall within normal adult ranges
- Baseline OH in the Elderly
- Positional SBP changes occur in 11 – 50% of patients > 65 years of age (Ooi 1997, Aronow 1988)
- Varies based on time of day and irrelevant of accompanying symptoms
Orthostatic Hypotension Take Home Point: At baseline, orthostatic vital signs are common and increases in frequency with age.
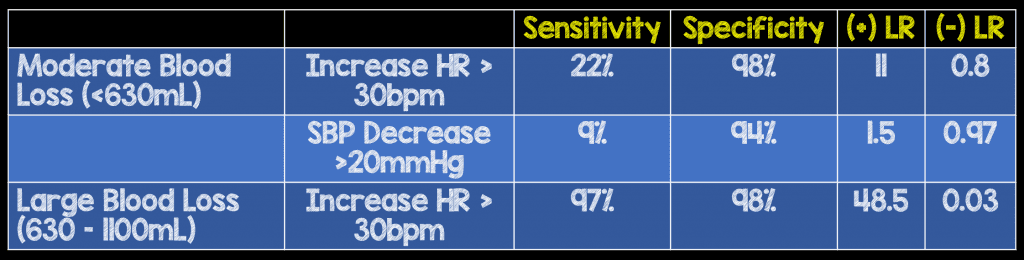
Orthostatics in Blood Loss
Witting MD et al. Defining the positive tilt test: a study of healthy adults with moderate acute blood loss. Ann Emerg Med 1994; 23(6): 1320-3. PMID: 8198307
What they did: Measured postural BP and HR changes after blood donation (450 ml) by healthy volunteers
McGee S et al. The rational clinical examination. Is this patient hypovolemic. JAMA 1999; 281(11): 1022-9. PMID: 10086438
Orthostatics in Non-Blood Volume Loss (i.e. vomiting, diarrhea)
Johnson DR et al. Dehydration and orthostatic vital signs in women with hyperemesis gravidarum. Acad Emerg Med 1995; 2(8): 692-7. PMID: 7584747
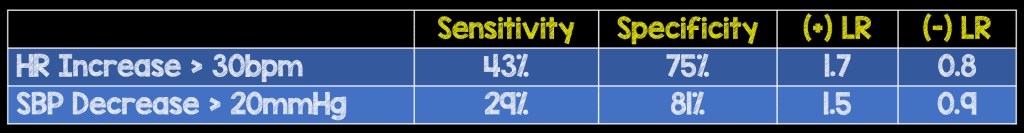
Orthostatic Hypotension Take Home Point: Orthostatic measurements had poor sensitivity for diagnosing moderate blood loss or significant dehydration. Performance characteristics were improved in large blood loss but, these patients are unlikely to be missed
Orthostatic Symptoms
Question: If the utility of the vital sign changes with position aren’t useful, what about simply using symptoms (I.e. the patient feels lightheaded when they stand.)?
Moderate volume loss: symptoms have limited predictive value
Severe volume loss (McGee 1999)
- Excellent performance characteristics of inability to stand for vital signs to be measured
- Sensitivity: 97%
- Specificity: 98%
- (+) LR = 48.5
- (-) LR = 0.03
- However, likely that diagnosis of severe volume loss can be made without this test
Orthostatic Vital Signs + Serious Outcomes
Question: Are the presence of abnormal orthostatic vital signs associated with 30-day serious outcomes in older adults presenting with syncope?
Abnormal orthostatic vital signs or symptoms are not associated with an increased risk of adverse outcomes at 30-days. (White 2019)
Odds Ratio for Serious Outcomes: 1.05 (95% CI 0.62 – 1.10)
Summary: Based on the limited available evidence, it’s unlikely orthostatic vital sign measurement can be used to determine which patients have volume loss and which do not. The baseline prevalence of orthostatic vital signs is common and patients will not always develop orthostatic vital signs in response to volume loss. Therefore, there will both be patients who are orthostatic by numbers without volume loss and there will be patients with volume loss who are not orthostatic by numbers. Symptoms, with the exception of inability to stand to have orthostatics performed, are not useful either. Finally, there doesn’t appear to be an association between the presence of orthostatics after syncope and adverse outcomes.
Bottom Line: Based on the low overall sensitivity of orthostatic vital sign measurements, they should not be used to influence clinical decision making.
References:
- Skinner JE et al. Orthostatic heart rate and blood pressure in adolescents: reference ranges. J Child Neuro 2010; 25(10): 1210-5. PMID: 20197269
- Stewart JM. Transient orthostatic hypotension is common in adolescents. J Pediatr 2002; 140: 418-24. PMID: 12006955
- Ooi WL et al. Patterns of orthostatic blood pressure change and the clinical correlates in a frail, elderly population. JAMA 1997; 277: 1299-1304. PMID: 9109468
- Aronow WS et al. Prevalence of postural hypotension in elderly patients in a long-term health care facility. Am J Cardiology 1988; 62(4): 336-7. PMID: 3135742
- Witting MD et al. Defining the positive tilt test: a study of healthy adults with moderate acute blood loss. Ann Emerg Med 1994; 23(6): 1320-3. PMID: 8198307
- McGee S et al. The rational clinical examination. Is this patient hypovolemic. JAMA 1999; 281(11): 1022-9. PMID: 10086438
- Johnson DR et al. Dehydration and orthostatic vital signs in women with hyper emesis gravidarum. Acad Emerg Med 1995; 2(8): 692-7. PMID: 7584747
- White JL et al. Orthostatic vital signs do not predict 30 day serious outcomes in older emergency department patients with syncope: A multi center observational study. Am J Emerg Med 2019. PMID: 30928476
Post Peer Reviewed By: Salim R. Rezaie (Twitter: @srrezaie)



