 Background: Emergency intubation in the ED is a potentially life-saving procedure in critically ill patients, but does have risks associated with it as we have discussed before on this blog. The authors of the study we are going to review today described a first-attempt intubation success (FPS) rate in the ED to be 85%, despite new technologies such as video laryngoscopy [2]. Successful endotracheal intubation on the initial attempt is vital as it reduces the likelihood of adverse events. Use of the bougie as the primary intubation approach may increase FPS but it is typically reserved as a rescue device only after failed intubation attempts. This is the first randomized controlled trial comparing the bougie vs endotracheal tube + stylet (ETT + stylet) in ED patients with at least 1 characteristic predictive of difficult intubation. The trial is titled the Bougie use in Emergency Airway Management (BEAM) trial.
Background: Emergency intubation in the ED is a potentially life-saving procedure in critically ill patients, but does have risks associated with it as we have discussed before on this blog. The authors of the study we are going to review today described a first-attempt intubation success (FPS) rate in the ED to be 85%, despite new technologies such as video laryngoscopy [2]. Successful endotracheal intubation on the initial attempt is vital as it reduces the likelihood of adverse events. Use of the bougie as the primary intubation approach may increase FPS but it is typically reserved as a rescue device only after failed intubation attempts. This is the first randomized controlled trial comparing the bougie vs endotracheal tube + stylet (ETT + stylet) in ED patients with at least 1 characteristic predictive of difficult intubation. The trial is titled the Bougie use in Emergency Airway Management (BEAM) trial.
What They Did: This was a single center, randomized clinical trial of consecutive patients, requiring orotracheal intubation with a Macintosh laryngoscope blade, comparing bougie first intubation vs ETT + stylet first intubation among patients with difficult airways undergoing emergency intubation performed by ED physicians.
Patient positioning, preoxygenation strategy, use of neuromuscular blockade (i.e. rapid sequence intubation), cricoid pressure, choice of Macintosh laryngoscope, and whether to view the video screen was all up to the emergency physician.
Outcomes:
- Primary: FPS in patients with at least 1 difficult airway characteristic (i.e. body fluids obscuring laryngeal view, airway obstruction or edema, obesity, short neck, small mandible, large tongue, facial trauma, or need for cervical immobilization)
- FPS was defined as successful endotracheal tube placement with the first device passed (bougie or endotracheal tube + stylet) during the first laryngoscope insertion
- Secondary:
- FPS in all patients
- FPS success without hypoxemia
- First attempt duration (i.e. time elapsed between insertion and removal of the laryngoscope blade from the patient’s mouth)
- Esophageal intubation
- Hypoxemia (i.e. SpO2 <90% or if the attempt began with a saturation <90%, and absolute decrease in desaturation of >10%)
Inclusion:
- Adult patients ≥18 years of age
- Emergency orotracheal intubation in the ED
- Use of a Macintosh laryngoscope blade (Standard geometry blade)
Exclusion:
- Prisoners
- Pregnant patients
- Known distortion of upper airway or glottic structures (i.e. angioedema, epiglottitis, laryngeal mass, or malignancy)
- Use of hyperangulated laryngoscope
Results:
- 757 patients randomized to Macintosh laryngoscope blade intubation for respiratory arrest, difficulty breathing, or airway protection
- 380 of the patients randomized had at least one difficult airway characteristic
- Bougie 1stIntubation = 381 patients (198 had a difficult airway characteristic)
- ETT + Stylet 1stIntubation = 376 patients (182 had a difficult airway characteristic)
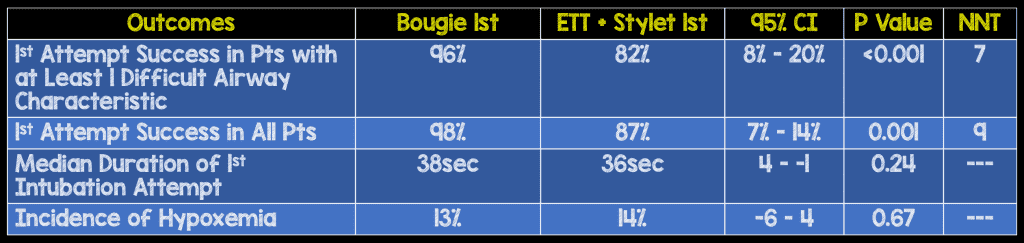
- No difference between groups for any intubation related complications including pneumothorax, aspiration, dental trauma, direct airway trauma, or esophageal intubation
Strengths:
- The study asks a clinically important question
- Randomization was adequately performed
- Data was collected in real time with the use of a stopwatch, increasing accuracy of times recorded
- Reporting of FPS was adjudicated by an investigator who retrospectively reviewed video of the captured intubation on motion-activated, ceiling mounted cameras
- A trained and blinded abstractor reviewed final postintubation chest x-rays to determine the presence of pneumothorax
- Individual physician’s intubation abilities were analyzed post hoc to account for clustering by physician as a physician’s abilities to intubate could affect FPS
- An interim analysis evaluating futility was completed at the midpoint of the trial
- Adherence to the randomized allocation was 98% in the bougie group and 92% in the ETT + stylet group
- Both groups were well balanced in terms of patient characteristics and clinical indications for intubation
Limitations:
- Single institution study where bougie 1stintubation is a common practice. This may not be generalizable to all institutions not as comfortable with the use of the bougie.
- Difficult airway features were determined by the intubating physician subjectively post intubation, but this was performed immediately after intubation minimizing recall bias
- For obvious reasons physicians and researchers could not be blinded as to which device was being used for intubation
- Patients intubated with hyperangulated laryngoscopes were excluded, therefore the results of this study are not to be applied for these devices
Discussion:
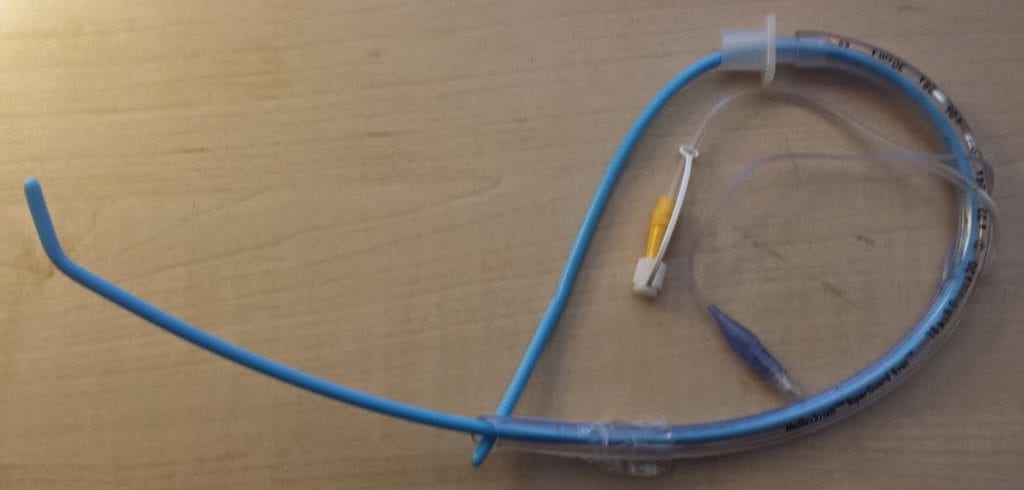
- Interestingly, in the bougie group, a bougie was passed into the trachea and if successful, an assistant loaded the endotracheal tube over the bougie and ultimately passed through the vocal cords. In the environments I work in, having an assistant is a luxury that’s frequently absent. This is where a pre-loaded bougie with an ETT, using a Kiwi grip becomes very useful (See image below).
- In their exploratory analysis, the bougie appeared to be superior compared to ETT + stylet for FPS in patients with cervical in-line immobilization (100% vs 78%), obese patients (96% vs 75%), and patients with incomplete glottic views on laryngoscopy (97% vs 60%)
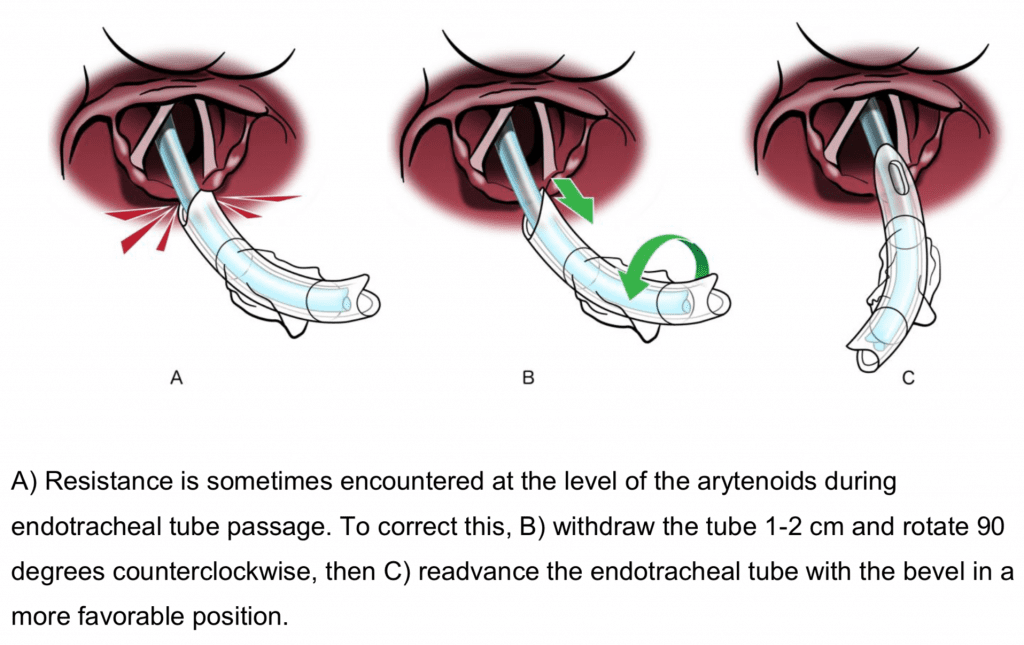
- 31 patients or 7% of the intubations with bougie met resistance from the arytenoid cartilages,but a simple maneuver with the ETT overcame this (see figure below)
Author Conclusion: “In this emergency department, use of a bougie compared with an endotracheal tube + stylet resulted in significantly higher first-attempt intubation success among patients undergoing emergency endotracheal intubation. However, these findings should be considered provisional until the generalizability is assessed in other institutions and settings.”
Clinical Take Home Point: Although, the results of this trial still need to be validated in other ED settings, use of bougie first instead of as a rescue device when using a standard geometry blade should be strongly considered.
References:
- Driver BE et al. Effect of Use of a Bougie vs Endotracheal Tube and Stylet on First-Attempt Intubation Success Among Patients With Difficult Airways Undergoing Emergency Intubation: A Randomized Clinical Trial. JAMA 2018. [Epub Ahead of Print]
- Brown CA et al. Techniques, Success, and Adverse Events of Emergency Department Adult Intubations. Ann Emerg Med 2015. PMID: 25533140
For More Thoughts on This Topic Checkout:
- Rory Spiegel at EMNerd (EMCrit): The Peculiar Case of the Parallel Pathways
- Simon Carley at St. Emlyn’s Blog: JC – Don’t Blame it on the Bougie
- Terren Trott at 5 Minute Airway: BEAM Article with Brian Driver Interview
- Pulm CCM: Bougies for all Intubations Led to High Success Rates, Even on Difficult Airways
- Scott Weingart at EMCrit: Airway Update – Bougie and Positioning
- Justin Morgenstern at First10EM: Bougie is Better
- Alex Chen at Journal Feed: Bougie vs Stylet – The BEAM Trial
- Ken Milne at The Skeptics Guide to Emergency Medicine: SGEM#271 – Bougie Wonderland for First Pass Success
Post Peer Reviewed By: Anand Swaminathan, MD (Twitter: @EMSwami)



