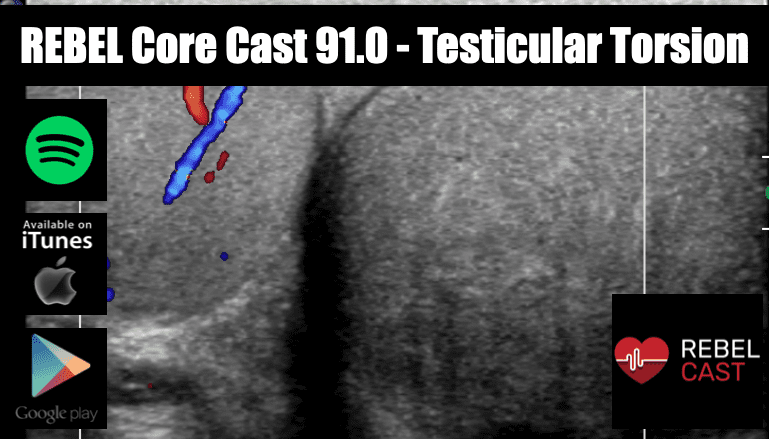
REBEL Core Cast 91.0 – Testicular Torsion
Take Home Points Consider the diagnosis of testicular torsion in all patients with acute testicular pain Testicular torsion is a surgical emergency that requires immediate urologic consultation to increase the rate of tissue salvage. History, physical examination and ultrasound are …